4 - Personal Protective Equipment (PPE): Respiratory Protective Equipment (RPE)
In addition to PPE used for Standard Infection Control Precautions, appendix 15 of the NIPCM outlines what type of PPE and RPE you will need to wear for infections spread by different transmission routes.
Gloves
Gloves are a single-use item and should be donned immediately prior to exposure risk and should be doffed immediately after each use or upon completion of a task.
Gloves should:
- be worn when exposure to blood, body fluids, (including but not limited to secretions and/or excretions), non-intact skin, lesions and/or vesicles, mucous membranes, hazardous drugs, and chemicals for example cleaning agents, is anticipated/likely
- never be worn inappropriately in situations such as to go between residents, move around a care area, work at IT workstations
- be changed if a perforation or puncture is suspected or identified
- be appropriate for use, fit for purpose and well-fitting
- not be worn as a substitute to hand hygiene
- never be decontaminated with ABHR
Resources
 For appropriate glove use and selection see the flowchart poster which may be printed off and placed in the care home.
For appropriate glove use and selection see the flowchart poster which may be printed off and placed in the care home.
![]() Further information can be found in the Gloves literature review.
Further information can be found in the Gloves literature review.
Aprons/gowns
An apron should be worn when caring for residents known or suspected to be colonised/infected with antibiotic resistant bacteria including contact with the resident’s environment.
Plastic aprons should be used in care home settings for protection against contamination with blood and/or body fluids.
A fluid repellent gown should be used if excessive splashing or spraying is anticipated.
A full body fluid repellent gown should be worn when conducting AGPs on residents known or suspected to be infected with a respiratory infectious agent.
![]() Further information can be found in the Aprons/Gowns literature review.
Further information can be found in the Aprons/Gowns literature review.
Eye/face protection
Eye and face protection should be used in combination with:
- a fluid resistant Type IIR surgical mask when caring for symptomatic residents infected with droplet transmitted infectious agents
- a fluid resistant FFP3 respirator when caring for symptomatic residents infected with an airborne transmitted infectious agent
Eye/face protection should be worn:
- by all of those in the room if potentially infectious AGPs are conducted
- for the care of residents with novel infectious agents including pandemic influenza
 Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Surgical masks
A Type IIR fluid resistant surgical mask (FRSM) should be worn when caring for a resident with a suspected/confirmed infectious agent spread by the droplet route.
FRSMs should be worn (where tolerated) by residents with suspected/confirmed infectious agents spread by the droplet or airborne routes, as a form of source control and should meet type II or IIR standards.
 Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Respiratory Protective Equipment (RPE)
PPE should still be used in accordance with SICPs when using respiratory protective equipment (RPE). See Chapter 1.4 for PPE use for SICPs.
The use of FFP3s is governed by health and safety regulations and they must be fit tested to the user to ensure the required protection is provided.
The Health and Safety Executive (HSE) provides information regarding fitting and fit checking of RPE.
Respiratory Protective Equipment (RPE), for instance FFP3 and eye/face protection, should be considered when:
- a resident is admitted or develops a known/suspected infectious agent/disease spread wholly by the airborne route
- carrying out AGPs on residents with known/suspected infectious agent spread wholly or partly by the airborne or droplet route
FFP3 respirators
It is an HSE requirement that staff who need to wear an FFP3 respirator must be fit tested.
FFP3 respirators should not be worn by staff who are not trained in their use or who have not been fit tested.
All FFP3 respirators must be:
- fit tested (by a competent fit test operator) on all staff who may be required to wear a respirator to ensure an adequate seal/fit according to the manufacturers’ guidance
- fit checked (according to the manufacturers’ guidance) every time a respirator is donned to ensure an adequate seal has been achieved
- single-use (disposable) and fluid resistant
- compatible with other items of PPE and worn in accordance with manufacturer’s instructions. Prescription eyeglasses and contact lenses should not be considered a form of eye/face protection
- put on before entry into the resident’s room and removed in a safe area once outside the resident’s room
- changed after each use
Signs that a change in respirator is required include:
- breathing becomes difficult
- the respirator is wet or moist
- the respirator is damaged
- the respirator is obviously contaminated with body fluids such as respiratory secretions
Resources
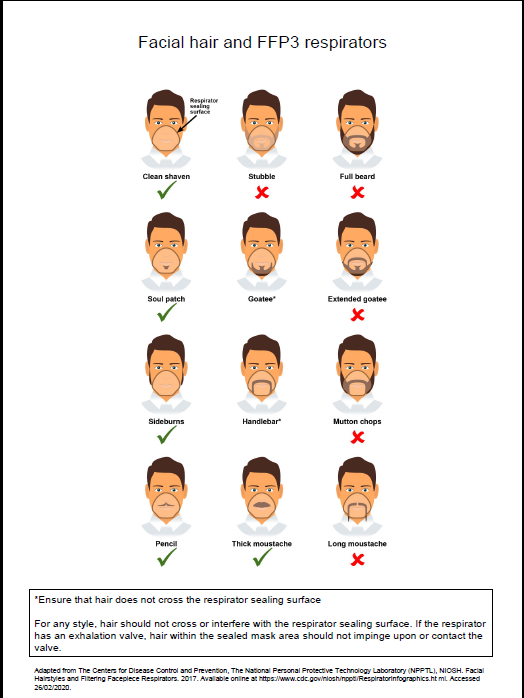
 A poster containing information on compatibility of facial hair and FFP3 respirators can be used when fit testing and fit checking.
A poster containing information on compatibility of facial hair and FFP3 respirators can be used when fit testing and fit checking.
![]() Further information regarding fitting and fit checking of respirators can be found from the Health and Safety Executive
Further information regarding fitting and fit checking of respirators can be found from the Health and Safety Executive
Aerosol Generating Procedure (AGP)
An AGP is a medical procedure that can result in the release of airborne particles from the respiratory tract and is associated with an increased risk of transmission when treating someone who is suspected or known to be suffering from an infectious agent transmitted wholly or partly by the airborne or droplet route.
The most common AGPs undertaken in the Care Home Setting are Continuous Positive Airway Pressure Ventilation (CPAP) or Bi-level Positive Airway Pressure Ventilation (BiPAP) or tracheostomy procedures (insertion or removal) and open suctioning beyond the oro-pharynx.
The full list of medical procedures that have reported to be aerosol generating and are associated with an increased risk of respiratory transmission can be found in appendix 16.
A poster is also available on PPE when undertaking AGPs within health and social care settings.
Rooms should always be decontaminated following an AGP. Clearance of infectious particles after an AGP is dependent on the ventilation and air change within the room. In an isolation room with mechanical ventilation 10-12 air changes per hour (ACH) a minimum of 20 minutes is required; in a side room with 6 ACH this would be approximately one hour.
It is often difficult to calculate air changes in areas that have natural ventilation only, meaning no mechanical ventilation. Natural ventilation, particularly when reliant on open windows can vary depending on the climate. An air change rate in these circumstances has been agreed as 1-2 air changes/hour.
Rooms should always be decontaminated following the completion of an AGP. Regardless of the number of air changes, a period of 10 minutes should pass to allow larger droplets to settle before the room can be cleaned. Staff are required to wear the appropriate PPE until the fallow time has been met.
Resources
![]()
For further information on fallow times refer to Table 1 in Appendix 16.
 Further information can be found in the literature reviews aerosol generating procedures, Respiratory Protective Equipment (RPE), Personal Protective Equipment (PPE) for High Consequence Infectious Diseases (HCID)
Further information can be found in the literature reviews aerosol generating procedures, Respiratory Protective Equipment (RPE), Personal Protective Equipment (PPE) for High Consequence Infectious Diseases (HCID)
Post AGP fallow time (PAGPFT)
Time is required after an AGP is performed to allow the aerosols still circulating to be removed/diluted. This is referred to as post AGP fallow time (PAGPFT) and is a function of the room ventilation air change rate.
The post aerosol generating procedure fallow time (PAGPFT) calculations are detailed in appendix 16. It is often difficult to calculate air changes in areas that have natural ventilation only.
If the area has zero air changes and no natural ventilation, then AGPs should not be undertaken in this area.
The duration of AGP is also required to calculate the PAGPFT and clinical staff are therefore reminded to note the start time of an AGP. It is presumed that the longer the AGP, the more aerosols are produced and therefore require a longer dilution time. During the PAGPFT staff should not enter this room without FFP3 masks. Other residents, other than the resident on which the AGP was undertaken, should not enter the room until the PAGPFT has elapsed and the surrounding area has been cleaned appropriately. As a minimum, regardless of air changes per hour (ACH), a period of 10 minutes should pass before rooms can be cleaned. This is to allow for the large droplets to settle. Staff should not enter rooms in which AGPs have been performed without airborne precautions for a minimum of 10 minutes from completion of AGP. Airborne precautions may also be required for a further extended period of time based on the duration of the AGP and the number of air changes. Cleaning can be carried out after 10 minutes regardless of the extended time for airborne PPE.
Contact your local HPT/IPCT if further advice is required.
 Read the RPE literature review to find out more about why we do things this way for respiratory protective equipment.
Read the RPE literature review to find out more about why we do things this way for respiratory protective equipment.
Use of FFP3 respirators
- Where staff have concerns, they may choose to wear an FFP3 respirator rather than a fluid-resistant surgical mask (FRSM) when providing patient care, provided they are fit tested. This is a personal PPE risk assessment.